Неординарный медицинский опыт к рутинным проблемам в США .

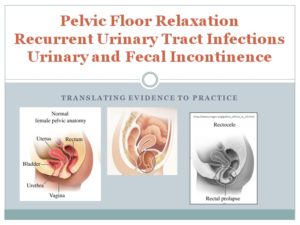
Estimate: Profound Pelvic organ prolapse (POP) affects 14% and urinary tract infection 40% (UTI) of women at some point in their lives and are important problems. The USA performs approximately 200,000 pelvic prolapse surgical procedures per year; in the US it is 20% of women who will have surgery for POP or stress urinary incontinence before the age of 80 (Wu, Matthews, Conover, Pate, & Jonsson Funk, 2014).
Note that isn’t how many HAVE some POP, that is how many agree to show up for surgery!
One in ten suffer from fecal incontinence (Cichowski, Dunivan, Rogers, & Komesu, 2014).
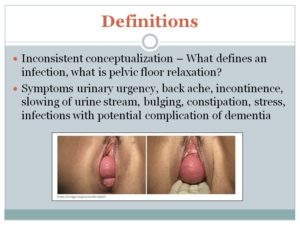
In these pictures one can see that certain parts of the bladder will not empty because water does not flow uphill and a contraction at the base of the bladder will be minimally effective in forcing urine out and the stream slows until in severe cystocele it becomes difficult to begin a stream. In the rectocele part of the feces remains in the pocket created by laxity in the vaginal wall. This amount of stool becomes harder as water is absorbed from the rectal wall. Once this forms a hard ball, it blocks the exit of the next bowel movement. This impaction can be complete or partial, but disrupts and irritates the entire system.
The difference between a urine specimen diagnosed ‘infection’ and actual infection — recent research demonstrates that organisms can invade the mucous layer of the bladder and evade detection in urine, but later when they become activated to be more virulent, they cause symptoms again.
On paper: “Positive urine culture in the presence of symptoms is the cornerstone of diagnosis of UTI and should be performed along with ultrasound assessment of post-void residual (PVR) in all women presenting with POP and UTI.” (but that almost never happens)
PVR over 30 mL is an independent risk factor for UTI, although no specific association with POP and UTI has been demonstrated” (Hamid & Losco, 2014).
(In most US clinics this woman would be fully dressed at a urologist office and have someone put an ultrasound to her upper pubic area while holding her pants down just a little bit, and declare that she has a PVR of zero. – thus “there is no specific association of POP and UTI” in meta-analysis work.)
Prescribing anti-biotics, as promoted through accepted guidelines, is quick and easy, yet we know, also harmful to these women and is a challenge to an International Action Plan for Combating Antibiotic-Resistant Bacteria . Treatment of Urinary Tract Infection Guidelines were originally based on research with younger women (Geerlings, Beerepoot, & Prins, 2014; Lindsay E. Nicolle, 2002)
A recognition that cooperation from the population of older women suffering from recurrent UTI, will be needed, to prevent or decelerate the rapid rise of antibiotic resistant organisms (Nami et al., 2015) Most women do not tell their providers of their struggles unless asked.
1/3 of people treated with antibiotics come to harm (Beveridge 2011) disturbance of the gastrointestinal tract in individual women.
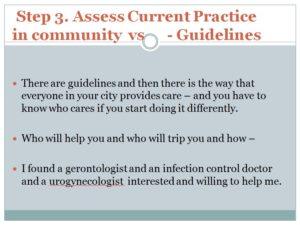
Guidelines and practice of the care for older women with UTI has predominantly resulted from expert opinion based on inductive reasoning, with reviews on research that focused on positivist variables and criteria, most of which was conducted with younger women (Grigoryan, Trautner, & Gupta, 2014; National Guideline Clearinghouse (NGC), n.d.-a, n.d.-b, n.d.-c, n.d.-d; L. E. Nicolle & AMMI Canada Guidelines Committee*, 2005).
Probiotics can improve vaginal heath so that pathogens are less able to colonize this area and have been shown to be effective in UTI with pelvic organ prolapse with less antibiotic resistance (Beerepoot et al., 2012; Darouiche & Hull, 2012; Vera, Juárez, Wiese, & Nader-Macías, 2014).
252 postmenopausal women with recurrent UTIs randomized -taking part in a double-blind noninferiority trial to receive 12 months of prophylaxis with trimethoprim-sulfamethoxazole, 480 mg, once daily or oral capsules containing 109 colony-forming units of Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14 twice daily.
Case- I had a patient who lost 40 pound in one year and had no idea why. She had been given 20 rounds of antibiotic by her previous doctor in one year. She had not been educated about probiotics. She had her intestines restored with enzyme and probiotic recommendations and then was put on Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14 twice daily, along with external application of a pea size amount of antibacterial cream alternating with antifungal cream and estrogen cream.

(for article not to be read during lecture- oral highlight of slide only) Relevant randomized controlled trials and published reviews and guidelines in English were identified through a search of PUBMED, professional journals, and review of references in articles of merit throughout the fall of 2010. The search terms included geriatric UTI, complicated UTI, guidelines, menopause & urinary tract infection, recurrent urinary tract infection, recurrent UTI, cystitis, probiotics, Lactobacillus reuteri, pelvic organ prolapse, post void residual, hyaluronic acid, urinary pH, antibiotic resistance, cystocele, estrogen and UTI, patient education, cranberry, trabeculation, pessary, fecal incontinence, pelvic floor physical therapy. Combinations of elderly and geriatric and postmenopausal were coupled with other terms.
Excel spreadsheets of probable patient loads and codes to model income.
Professional organizations were joined on local and national levels: SUNA, Simon Foundation, POPS Association, NPWH, WOCN.
Medical license board conversations to make sure no one was practicing outside their license.
American Urogynecologic Society Prolapse Consensus Conference Summary Report (just released 2018) 70 seconds.
The Innovating for Continence Conference Series is a unique, international, biennial conference for engineers, physicians, nurses, people with incontinence and their caregivers, academics, industry executives, and those with a passion for increased development of creative and efficacious products for the management of incontinence. We also have this near my house for Bowel Disorders such as Crohn’s at Vanderbilt University. These types of conferences are wonderful resources for all involved.
It is important that we understand that women want to hear a message of hope, encouragement and personal effort from providers (Cichowski, Dunivan, Rogers, & Komesu, 2014).
Most of my patients would be referred to see me with multiply drug resistant organisms in their urine, in their stool, in wounds on their labia etc. Learning about infective organisms and how to stay safe against them was a high priority! I use silver on my hands daily.
Silver Nanoparticles are now considered a viable alternative to antibiotics and seem to have a high potential to solve the problem of the emergence of bacterial multidrug resistance In particular, silver nanoparticles (AgNPs) have attracted much attention in the scientific field (Franci et al., 2015).
We purchased this and it came with a toilet that measured urine stream as the patient urinated, documenting if the patient had slow stream. Then it measured patient urine volume, and I used a simple dip-stick to test the urine for pH and nitrates etc. Then we used this equipment to perform ultrasound for post-void residual.
The company that we purchased equipment from trained me in how to use an ultrasound that provided pictures in two planes. Its computer combined those images to provide post void residual volume in cc. This helped me have a better concept of actual bladder placement.
With this particular ultrasound I could see the shape of the bladder as well- it gave me more than just a read-out of volume.

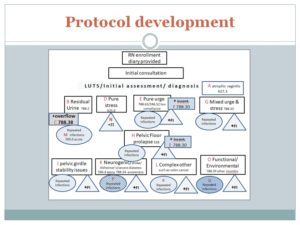
Planning for what tests and diagnosis would lead to what further tests, numbers of visits etc.
This is the global explanation- no details/ translation of slide not needed.
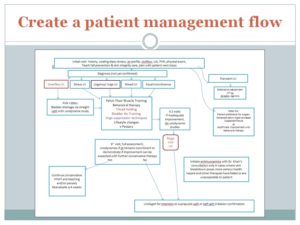
Again the details do not need to be translated.
“This is my messy and crazy but original unedited work in trying to sort out how many protocols I would need to document.
I made up a page of instructional protocols for ideal care for each diagnostic code, with tests and protocols to be offered, so that the doctor and I could decide if I would treat or refer at each junction.
We will not dissect this chart, but we might look at one box that says: Atrophic vaginitis as an example of bringing research to clinical practice- Almost all of my patients have this because a majority were being referred in from a geriatrics doctor.
They could be treated with a new medication Ospemifene for dry vaginal vault, or by standard estrogen creams or the new ring pessary with timed release estrogen- called Estring. The doctor had to decide that we could treat with any of these, because in his practice- before working with me- he NEVER treated ANY of his patients at all and in fact he would take all patients off of any estrogen other doctors had put them on, as soon as they became his patient. But I showed him research which demonstrated that Estring reduced urinary tract infections without raising risks of stroke, and reluctantly he allowed me to begin using them. (Perrotta, Aznar, Mejia, Albert, & Ng, 2008) (Raz, 2011) We had to be in agreement on the treatments we were planning.
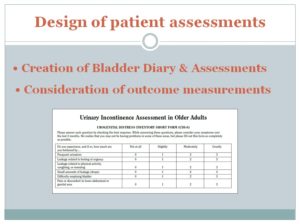
Use a few common assessment tools — even if you don’t like them very much, because to do research, you need to be able to compare apples to apples. This form was in universal use but had little true ‘validation’.
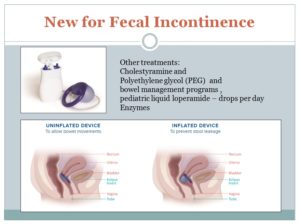
There is a new treatment being prescribed in a facility 2 hours from my home. The Eclipse System (Richter et al., 2015).
I used medication oriented treatments listed in upper right along with diet reviews, but I do not have time today to review those treatments except to say that almost all my patients had difficulty with bowel movements and PEG has been shown to be very useful and non-harmful (Dipalma, Cleveland, McGowan, & Herrera, 2007) .
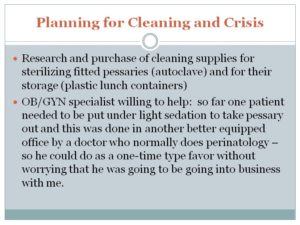
Pessaries are a main component of my clinical care. (Jones & Harmanli, 2010) The slide shown of a serious cystocele might respond perfectly to a pessary. I had many patients as severe and of course many who had no visible sign outside their bodies, and when we could get a good fit with the pessaries, then they had resolution of symptoms.
I learned to fit cervical caps years before while doing a cervical cancer prevention project. For this I had to learn from another provider and I had to learn from my patients. I learned from another provider that the Hodge is much more useful than what it says on the label. It folds in half so insertion into the body is easy and tiny, then it springs open, to hold the vaginal vault and the rest of the contents of the abdomen, in much better alignment.
Most of my peers use the rings most often, or the gelhorn because that is what they were taught to use, but in my patients the rings usually fell out with any strain, whereas the square part of the Hodge lodges against the pubic bone to prevent slipping. Removal of the Gelhorn is a real trial for the patients. Most women can get the Hodge in and out on their own. A recent article on Trimo-San said it wasn’t needed (Meriwether et al., 2015), but in my older patients it was definitely needed, and in my younger patients not so much…once again, we compare apples with oranges in meta-analysis.
One of my patients had very serious heart problems and was in her 80s so she was not a good surgical candidate but she had at least 4 inches of rectocele outside of her body. I used a size 5 Hodge and it tucked up beautifully. She was so grateful! I had her come in once a month to clean it and to check her for erosions because we could not use estrogen of any kind for her.
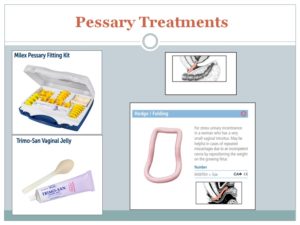
This is available via Amazon and is disposable. Significant improvement in the quality of life in women treated with a novel disposable intravaginal device for stress urinary incontinence. Ziv E, et al. The chart showing response to this pessary is probably similar to what we would find in other pessaries, but the style of this one may predispose to more or less pressure points and vaginal erosion areas. That remains to be researched.
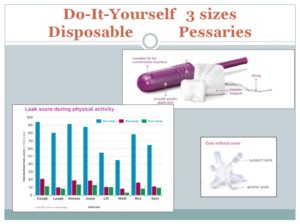
Also available through Amazon – Uresta is more expensive and is washable, instead of disposable. It is to improve urinary incontinence – mild relaxation.
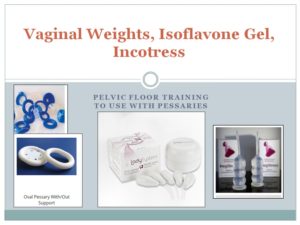
Soy isoflavone vaginal gel helps create a healthier vaginal pH which helps benign flora compete and reduce detrimental flora. (Lee et al., 2018)
Impressa (Farrell, Baydock, Amir, & Fanning, 2007) pessaries (Jones & Harmanli, 2010) Ring pessary prospective (Ding et al., 2016)

Vaginal cones, (Ayeleke, Hay-Smith, & Omar, 2015) (Golmakani, Khadem, Arabipoor, Kerigh, & Esmaily, 2014) oval pessaries, assorted strengths
Incostress by C&G, a combination of vaginal cone and pessary is the large clear looking piece of silicone.
After changing local practice, publications are needed to change national practice and international conferences like this to help improve the lives of women world wide. Thank you.